AmSci Holiday Gift Guide
By The Editors
December 8, 2023
Science Culture Biology Communications Environment Scientists Nightstand
The holiday season is upon us, and if you’re looking for some gifts, we have an extensive list of STEM-related books to suggest for you! Even if you started early and you’re all done with your holiday shopping, books are great gifts for any time of the year. There are so many wonderful STEM books out right now, and this is just a small sampling. We’ve briefly reviewed some of our favorites.
For even more recommendations, check out some of our previous gift guides, too:
• 2022
• 2021
• 2020
• 2019
• 2018
STEM Books for Young Readers
(Suggested age ranges, where noted, are those provided by the publisher.)
Breaking the Mold: Changing the Face of Climate Science by Dana Alison Levy. Ages 8–12. Holiday House, 2023. $22.99.
In this book, Levy profiles 16 people, all of whom study different aspects of the Earth, animals, landscape, or climate. Each entry is compiled from personal interviews and has photos and infographics about the person’s work, making for a visually engaging read. These scientists are disabled; LGBTQ+; Black, Indigenous, or people of color (BIPOC); just starting out in the field; have years of work behind them; evangelical; and much more. There are climate change activists, volcanologists, botanists, and public health professionals—the diversity of areas of study is a real plus of this book, showing kids just how broad an area of science can be. These individuals are out in the field, in the lab, in the classroom, and around the world, working hard to make a difference.
They share stories of how they got into their field of interest, challenges or setbacks they experienced, what they’d like to see change in the world and in science, and frustrations they have with their work. The scientists put a personal spin on their work, reminding the reader that behind every researcher, there’s a story. At the end of the book there’s a section on nonscientists making a difference, along with DIY activities, a section on citizen science, and an extensive resources section.—Jaime Herndon
Brittanica’s Encyclopedia Infographica by Valentina D’Efilippo. Ages 10–14. Brittanica Books, 2023. $32.00.
Infographics are a wonderful tool: They make concepts visual, and have the power to convey a lot of information in a clear, succinct way—which is why I was really excited to see this book. Don’t be fooled by the age category: This oversized, colorful book provides an immersive experience for any reader, even adults. There are categories that include space; animals; land, sea, and sky; the living planet; the human world; and the human body. With 200 infographics to explore, readers will remain occupied for a while.
If you’re new to infographics, there’s even a section in the beginning of the book explaining how to read infographics and the information they present. It’s also a good refresher to anyone, reminding us to slow down and really take in the data presented.
Younger kids will enjoy the artwork and fun facts, but it’s older kids and adults who will get the most out of this book. I’m still exploring all the infographics, and my seven-year-old son is enjoying all the random facts he’s learning (and sharing with others). —Jaime Herndon
Can You See It? by Susan Verde, illustrated by Juliana Perdomo. (Ages 4–8). Abrams, 2023. $15.99.
A celebration of observation and attention to little details, Can You See It? offers poetic text from bestselling author Susan Verde, paired with Juliana Perdomo’s illustrations that have a bright, retro, Latin American style. The book makes a distinction between “looking,” which “shows me what is right in front of my eyes,” and “seeing,” which is more mindful and shows the reader more than what first meets the eye. For example, one can “look” at a tree, but when one slows down to "see," one observes life: “Signs of change and letting go, flowering and feeding, shading and sheltering. A place to call home.” Each spread introduces a new theme to observe: a tree, a city block, the sky, a friend, a family, oneself. With each theme, the book prompts the reader: “What can you see?” My two-year-old daughter loved answering this question, looking at the details of the illustrations. Older kids would also understand that they can answer this question with deeper observations beyond what is on the page, including their internal landscape, memories they have, and the world around them.—Katie L. Burke
The City Tree, by Shira Boss and illustrated by Lorena Alvarez. Ages 4–8. Clarion Books, 2023. $19.99.
This book honors urban trees by describing one special connection between a little girl, Dani, and the tree that is planted outside her apartment. The tree changes her soundscape, so that she is shielded from the street noise and instead, hears more birds. The tree also tells her about the weather: “Its leaves fluttering said breezy today, its branches bending said bundle up.” As readers follow Dani’s observations of the tree through various weather, times of day, and seasons—depicted in colorful, lively illustrations of city life—we see all the benefits it offers her and her neighbors. They, in turn, help care for the tree and its ecosystem. —Katie L. Burke
Feel the Force: Revealing the Physics Secrets that Rule the Universe by Mike Barfield. Ages 9–11. Laurence King Publishing, 2023. $19.99.
Feel the Force: Revealing the Physics Secrets that Rule the Universe is a captivating children's book that takes young readers on an exciting journey through the fascinating world of physics. Written by the award-winning British writer and cartoonist Mike Barfield, this book combines engaging storytelling with brightly colored illustrations to make complex scientific concepts accessible and fun for kids.
With a clear and playful narrative, the book introduces children to the fundamental forces of the universe, such as gravity, electromagnetism, and the strong and weak nuclear forces. It explores how these forces shape our everyday lives and the entire cosmos, from the orbits of planets to the behavior of tiny particles.
Readers will be enchanted by the colorful and interactive illustrations that help them visualize abstract concepts and hands-on experiments, and activities encourage them to explore the forces of physics in their own environment. Whether it's learning about the power of magnets or understanding why things fall, this book makes science come alive.
Feel the Force is a must-have for any budding scientist, providing a solid foundation in physics while sparking curiosity and a lifelong love of science. This book's engaging approach makes learning about the forces that govern our universe an unforgettable adventure for kids of all ages. —Nwabata Nnani

A Little Guide to Nature series: Hello Fungi and Hello Trees by Nina Chakrabarti. Ages 6–8. Laurence King Publishing, 2023. $10.99 each.
Nina Chakrabarti encourages her young readers not just to see trees, but to make friends with one in their neighborhood, say hello whenever passing, and notice its seasonal changes. Mushrooms are more ephemeral, but she advocates for close inspection, maybe drawing their portraits. Such a personal, anthropomorphic approach seems whimsical, but can evoke in children a connection to nature and a deeper sense of observation of the world around them. This Little Guide to Nature series includes rich spreads of illustrations mixed with brief, fun facts about the subject, in this case either trees or fungi. Young readers may delight in some of the less serious content, such as how some trees give off a stink to attract pollinators (female ginkgo trees smell of dog poo!) or how fungi such as the aptly named wolf farts distribute their spores with explosions. But in between, there is plenty of great introductory information about different kinds of trees or fungi, how they grow, where they live, the colors they take on, and a lot more. In some cases, the brief overview may leave readers with questions (such as how to mycorrhizal fungi help trees communicate with each other?) but hopefully that will encourage readers to delve further into more detailed sources. These pocket guides are colorful, fun introductions to much broader topics that could keep kids asking “why” for years.—Fenella Saunders
It’s Just Skin, Silly!, by Nina Jablonski and Holly Y. McGee. Ages 6–10. Catalyst Press, 2023. $18.99.
It's Just Skin, Silly! is a heartwarming children's book that tackles the important topic of diversity and acceptance with grace and simplicity. Written by anthropologist and paleobiologist Nina Jablonski and historian Holly Y. McGee, the book encourages young readers to celebrate differences and embrace the beauty of individuality.
Through delightful illustrations, the book gently teaches children that skin color is just one small part of who we are, and that it's what's inside that truly matters.
It's Just Skin, Silly! encourages kids to ask questions, learn about each other's cultures, and appreciate the richness of a diverse world. It promotes empathy and kindness, instilling in children the importance of treating others with respect and acceptance. This book is not just a source of education, but also a source of inspiration, reminding readers that our differences make the world a more exciting place. With its engaging narrative and vibrant illustrations, It's Just Skin, Silly! is a must-read for parents, teachers, and children alike, as it paves the way for a future built on love, understanding, and unity. —Nwabata Nnani
Lore of the Stars: Folklore & Wisdom From Above & Beyond, by Claire Cock-Starkey and Hannah Bess Ross. Ages 6–12. Wide Eyed Editions, 2023. $24.99.
The latest installment in a great series, this book is a gorgeously illustrated, oversized book that is filled with myths and folktales about the universe from around the world and through history. The Sun, stars, planets, cosmos, and much more are all in this book, with diverse stories about how the universe came to be and what elements of the cosmos represent and signify. There are creation stories about constellations, information about sky and weather deities in world mythology, and what mythology and folklore tell us about worlds beyond our own. The pictures are vivid and colorful, and the stories and snippets of information are perfect for diving into, even if you don’t have a ton of time. I will say there is such a variety of information on one page, sometimes about very different things, that for younger kids it can get a bit overwhelming because of the intensity of the illustrations and colors, combined with the text. —Jaime Herndon
My First Book of Electromagnetism by Eduard Altarriba and Sheddad Kaid-Salah Ferrón. Ages 8–16. Button Books, 2023. $17.99.
The long-running My First Book series has covered everything from microbes to quantum physics, and it never disappoints, with bright illustrations and engaging text. My First Book of Electromagnetism is a welcome addition to the series, tackling the history and physics behind the power of electricity that we all use every day. The book starts out by connecting electricity and magnetism, an association that kids might not make, and then explaining why the name electricity evolved from the ancient Greek word for amber. The introduction then moves on to some of Benjamin Franklin’s experiments on charging glass and amber rods by rubbing them with a silk handkerchief, and delves into how atoms are behind the formation of positive and negative charges. Simple experiments are detailed throughout the book, such as how to build an electroscope to measure the presence of an electric charge in an object, or how to build a homemade battery. The text explains how electric currents flow, and then connects that concept back to magnetism. After discussing the basics of magnetic poles and explaining what makes a material magnetic, we find out the history of the discovery that electricity generates magnetism and vice versa. Electromagnetism, the author explains, forms the basis of electric motors and electric generators, and electromagnetic waves are connected to light. The book is a great introduction to the topic for the curious reader around 8–11 years of age, depending on reading level, who wants to understand what happens when they flip on a light switch or turn on their computer. —Fenella Saunders
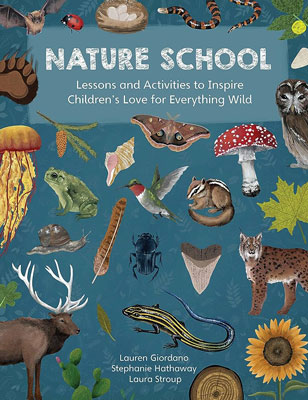
Nature School: Lessons and Activities to Inspire Children’s Love for Everything Wild, by Lauren Giordano, Stephanie Hathaway, and Laura Stroup. Ages 6–10. Quarry Books, 2023. $24.99.
I homeschool, and this book was a staple during our summer learning. It’s categorized for ages 6–10, but it can be used for older kids and even teenagers, with supplementation. The book covers five biomes: temperate forests, deserts, grasslands, seashores, and wetlands, and explores the plants and animals in each one. There are activities and arts and crafts, and the material is laid out in such a way that it’s easy to add supplemental material for older kids, and adapt it for younger ones. Topics include life cycles, ecosystems, climate and weather, and much more. I’m not a crafty person, so I especially liked how the activities and crafts didn’t always involve a ton of prep and clean up. I found the book to be well-researched and accessible, and it’s one we’ll be returning to again and again, in different ways. —Jaime Herndon
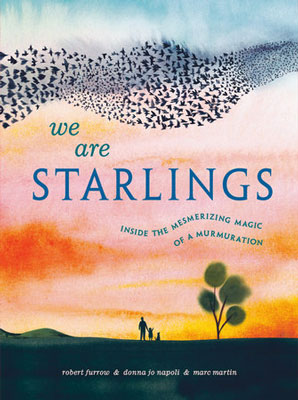
We Are Starlings: Inside the Mesmerizing Magic of a Murmuration, by Robert Furrow and Donna Jo Napoli, illustrated by Marc Martin. Ages 4–8. Random House Studio, 2023. $18.99.
My two-year-old picked this gorgeous book full of sunset colors off the library shelf, and was indeed, as the title promises, mesmerized. She rubbed her hands across the pages of the sweeping watercolor images and made sound effects for the birds flying across the pages: “Woaaaaah!” Among the stack of library books we brought home, this book was the one she asked for over and over again. The text gives simple, poetic explanations for how hundreds—or even millions—of starlings come together in flocks that move as if they are one organism. In doing so, they are able to better avoid a fearsome and quick predator, the peregrine falcon. “We find strength and safety in numbers,” the starlings say. “We find warmth in numbers.” But practicalities aside, flying in a murmuration is an incredible experience. One of the final pages opens out to a four-page spread, with the starlings having fun in great loops across the sky. Much older children than my daughter would also enjoy this poignant book; its target audience includes early readers who are a bit older. Adults will enjoy reading it out loud, too. I know I did. —Katie L. Burke
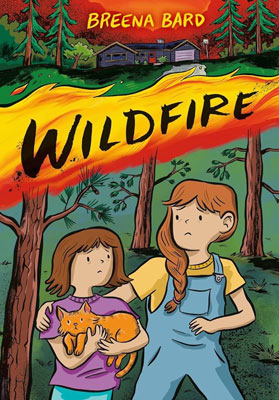
Wildfire by Breena Bard. Ages 8–14. Little, Brown Ink, 2023. $12.99.
I read this book in a single sitting because the story drew me in. The bright and vibrant art in Wildfire is a perfect complement to the story, too, making it a pure delight to read, despite the heavy themes of the story. Julianna loved living on her farm in rural Oregon and going to 4H. But when a wildfire destroys her home and kills her animals, she has to move to Portland. Some kids playing carelessly with fireworks are thought to be the cause of the fire, and Julianna realizes that she may know who those kids were. Her family starts becoming involved in climate change activism, but she’s not very interested—until an old friend who might have been involved with the fire moves to Portland. In order to heal, Julianna decides to join her family in their activism, and finds that each person can make a difference in their own way. I liked how Bard managed to weave in the arc of the fire and climate change, but also the arc of healing after trauma and channeling despair into action and hope. —Jaime Herndon
STEM Books for Adults
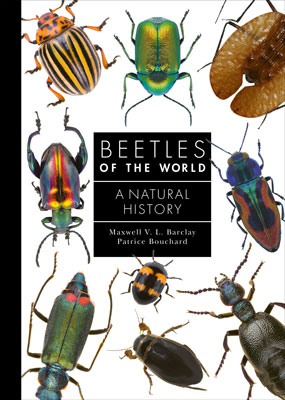
Beetles of the World: A Natural History by Maxwell V. L. Barclay and Patrice Bouchard. Princeton University Press, 2023. $29.95.
Although beetles make up about a quarter of known animal species and almost 400,000 species of beetles have been formally described, it is quite likely that their numbers are far greater. Any beetle book may call to mind the quip from British biologist J. B. S. Haldane, who famously stated that any creator must have had “an inordinate fondness for beetles” because there are so many. The authors of Beetles of the World definitely have an inordinate fondness for them; Barclay manages one of the world’s oldest collections of beetles at the Natural History Museum in London, and Bouchard has a similar role at the Canadian National Collection of Insects, Arachnids, and Nematodes. These two curators share their enthusiasm in this comprehensive, beautiful, and fun guide that details what makes a beetle a beetle, and explore their life cycle, fossil history, feeding habits, food webs, habitats (which are extremely varied), as well as their long relationship with humans. Beetles are crop pests, but are also pollinators and biological controls of other problems, such as weeds. They are eaten, worn as ornaments, feature in mythology, and are useful in some medicines. The majority of the book breaks the order Coleoptera (to which all beetles belong) into suborders and families, giving habitat, size, and diet for each, as well as some facts and lots of pictures. The range of beetle images might not make you inordinately fond of them, but it definitely provides the reader with a better appreciation of the vastness of this group of insects. —Fenella Saunders
A City on Mars: Can We Settle Space, Should We Settle Space, and Have We Really Thought This Through? by Kelly and Zach Weinersmith. Penguin Press, 2023. $30.00
Do you believe humans are destined to spread out into space, establishing settlements beyond Earth? It’s a polarizing question, with portions of the population living in—pardon the expression—totally different worlds. On one side there are the Trekkies and Musk-ovites who take it for granted that the arc of progress bends inevitably toward the stars. On the other, there is the vast segment that regards the notion of space outposts with either skepticism, or more likely, doesn’t think about it at all.
A City on Mars has a lot to offer both camps. For the true believers, the book lays out the excruciating challenges of life on Mars at a level of detail that enthusiasts rarely consider. Kelly Weinersmith is a biologist and Zach is a science-y cartoonist, creator of the clever “Saturday Morning Breakfast Cereal” series. They write with witty but relentless precision about everything from the scatological indignities of long spaceflights (beware the floating “brown trout”) to the grim prospects for new inhabitants on Mars, who are likely to live in windowless habitats buried beneath mounds of radiation-shielding rocks, struggling to grow plants in chemically hostile soil and treating every pregnancy as a genetic experiment.
For the skeptics, the Weinersmiths take a clear-eyed look at why people might decide to go anyway. The authors brush aside common but logically shaky arguments for settling on Mars, such as the idea that it could be a “Planet B” safe haven in case things go wrong here. (Earth would still be much more habitable than Mars even if we suffered runaway climate change, a giant asteroid impact, and nuclear war…all at once.) The rationale for space outposts may be couched in strategic or economic terms, but ultimately it more likely will boil down to personal impulse: “Because it’s awesome,” as the Weinersmiths put it.
Humans do a lot of things because they find them interesting and worthwhile, with pragmatic reasons arising only later. Building cities on other worlds may fall into this category. Regardless of motivation, A City on Mars offers an exceptionally thorough look at how we might do it, and at the consequences that would follow. The final third of the book is devoted mostly to the arcane yet crucial legal and political challenges of creating entirely new nation-states in the cosmic commons. Nobody wants planets populated with indentured servants, or tensions that lead to interplanetary warfare. One book cannot avert such possible futures, but thinking about them now surely makes them less likely. – Corey S. Powell
The Deserts of California: A California Field Atlas, by Obi Kaufmann. Heyday, 2023. $55.00.
This is the latest in Kaufmann’s California Lands Trilogy; his previous titles in the series include The Forests of California and The Coasts of California. This is not your typical field guide—none of them are. Clocking in at nearly 600 pages, this richly illustrated book is not only a guide but also a nature journal of sorts that includes history, geography, topography, and ecology of the deserts of California. Kauffman highlights national parks and monuments, providing illustrations and statistics, elevations and square mileage, and catalogs of the wildlife in each area he explores. But this is not merely a guidebook or documentation of geography: He also writes about the future of deserts in California, the general ecological and climate future, and the potential effect it has on the desert ecosystem. I don’t live in California and don’t have any plans to visit anytime soon, but this book, along with the others in the trilogy, is a joy to read. It’s chock-full of information about botany, wildlife, and other ecological aspects of California’s deserts, put together in an accessible, visual way. This approach helps to encourage a love of place, which is often the first step toward wanting to protect and preserve it. —Jaime Herndon
Entangled Life: The Illustrated Edition: How Fungi Make Our Worlds by Merlin Sheldrake. Random House, 2023. $40.00.
You might be familiar with the first edition of Sheldrake’s book Entangled Life, but even if you’ve already read that one, you won’t want to miss the new illustrated edition. Although it is abridged by the author, the photographs—more than 100 of them, in full-color—more than make up for the cut text. For true fungi lovers, I would recommend this book as a supplement to the first edition, so you get the bulk of the detailed text. But you won’t want to miss these (mostly) full-page photos that capture the minutiae of fungi, along with their vibrancy. Sheldrake’s passion for fungi and his ability to draw readers into the subject, even if they initially have less interest in it, is present throughout. The book makes the perfect addition to a STEM-lover’s coffee table. —Jaime Herndon
The Future of Geography: How the Competition in Space Will Change Our World by Tim Marshall. Scribner, 2023 $28.00.
This quirky book is best read as a coda to Kelly and Zach Weinersmith’s A City on Mars. Skip the first section (a rote history of astronomy and space exploration) and jump to the following discussion of space law—or, in the author’s term, “astropolitics.” Marshall, a veteran foreign-affairs reporter, zeroes in on gaping holes in the existing patchwork of space-related treaties and regulations. Whereas the Weinersmiths focus on issues related to future human exploration beyond Earth, Marshall flags the many challenges that are right here, right now.
The current mishmash of legal guidelines is already inadequate to deal with space junk and enormous satellite constellations like Starlink, he notes. There are also limited guardrails in place to prevent space-based warfare, which wouldn’t require a single shot fired: Jamming or hacking a nation’s military surveillance satellites could be a prelude to an attack, or could itself trigger a physical conflict on the ground. Marshall is predictably better at identifying problems than he is at proposing solutions. But he lucidly argues that the world needs robust new space agreements informed by past successes in areas like arms control and maritime law. As he writes, “Without laws, geopolitics—and now astropolitics—is a jungle.”—Corey S. Powell
Paint, Sweat, and Tears: 150 Days on the Appalachian Trail by Carolyn Matthews-Daut. MindStir Media, 2023. $28.95.
The Appalachian Trail (AT) has long intrigued me, and next year I’ll be hiking a short part of it. As part of my preparation, I’ve been reading everything I can about AT hikes, as well as books about the varying wildlife and ecology along the trail. I’ve also been striving to establish a daily nature journaling practice that includes sketches, and so I was drawn to this book (no pun intended!), which is a graphic travelogue/memoir about a through-hike. But it’s not just your typical hiking memoir: Matthews-Daut also draws her surroundings, the wildlife and fauna, and the landscapes along the trail, reminding the reader that hikers should never underestimate the natural world. She shares the emotional challenges of what a long-distance AT hike entails, the physical demands, and the camaraderie she encounters on the trail, all against an incredible natural backdrop.
Even if you aren’t a hiker, the vivid sketches and watercolor illustrations make this book a delight to read, immersing you in her travels. —Jaime Herndon
Sisterhood Heals: The Transformative Power of Healing in Community by Joy Harden Bradford. Ballantine Books, 2023. $28.00.
Sisterhood Heals is a compelling and empowering exploration of the healing power of female friendships and support networks. Drawing from her extensive expertise as a licensed psychologist and from her personal experiences, Joy Harden Bradford delves into the profound impact that sisterhood can have on women's mental and emotional well-being.
Readers are guided through the complexities of women's relationships, with a focus on the unique bonds between women. Bradford skillfully unpacks the challenges women often face, such as societal pressures, competition, and the stigma surrounding mental health. She also emphasizes the importance of creating safe spaces for vulnerability, self-compassion, and mutual growth within these relationships.
Practical strategies and tools for navigating difficult conversations, supporting one another during life's trials, and fostering resilience and mental health are just some of the topics Bradford addresses in the book. It is a heartfelt call to action, urging women to prioritize their own well-being, along with that of their fellow sisters.
Sisterhood Heals is a testament to the strength of women coming together and offering hope, encouragement, and a roadmap to fostering healthier, more fulfilling connections with the important women in their lives. —Nwabata Nnani
What’s Hidden Inside Planets? by Sabine Stanley with John Wenz. Johns Hopkins Wavelengths, 2023. $16.95.
For planets, as for people, there is a lot more going on that what you see on the surface. Look at our own Earth: The surface is slathered in water and oxygen, along with the ubiquitous carbon-based organisms soaking them in. What’s down below is totally different: A churning, silicate mantle cycles carbon and water, while deeper still, a liquid metal outer core generates a potent magnetic field that protects our atmosphere from being stripped away. Earth would not be its happy, vital self without all that soulful internal activity.
Stanley, a planetary scientist at Johns Hopkins University, approaches her topic with the generous enthusiasm of a nature guide taking visitors on a field trip. In this case, the “fields” are extreme environments where no human being could ever set foot—but with the aid of modern research techniques, we can tour them all the same. Following a classic “you are here” approach, Stanley begins by investigating Earth before moving on to the internal structures of other worlds.
And what worlds they are! Deep inside Saturn, a relentless rain of helium appears to heat the planet’s interior and to steal vast quantities of helium from the atmosphere above. Uranus and Neptune have even more exotic materials inside: a slow-motion hailstorm of diamonds (diamonds!) falling through high-pressure form of water called superionic ice, which is hot, black, and electrically conductive. The moons of the outer planets hold startling secrets as well. Several of them—most notably Jupiter’s Europa and Saturn’s Enceladus—have warm oceans hidden beneath their frozen exteriors. Those oceans are plausible habitats for alien life.
Sleuthing out such details is not easy, as Stanley deftly explains. On Earth, the deepest borehole extends just 7.6 miles; nobody has yet managed even to pierce the planet’s crust. Much of what we know about the mantle and core comes from studying how seismic waves pass through the planet. Seismometers on the Moon and Mars have provided some analogous insights there. For all other worlds, the available tools are more indirect, such as measurements of their masses, motions, and magnetic fields. And yet, despite these limitations, researchers have begun decoding the inner structures even of planets around other stars.
“I hope I’ve been able to portray how wondrous the inner worlds of planets are,” Stanley writes modestly near the end of her book. Hope achieved.—Corey S. Powell
Wild Girls: How the Outdoors Shaped the Women Who Challenged a Nation, by Tiya Miles. W.W. Norton & Co., 2023. $22.00.
Don’t let the slim appearance of this book fool you—there’s a lot here. Miles looks at various women who have changed America, and how the outdoors shaped them. The natural world provided them with a place that society couldn’t (or wouldn’t), and enabled them to nurture their independence, instincts, values, and personalities. Harriet Tubman, Louisa May Alcott, Sacagawea, Dolores Huerta, and many more, all found confidence and skills in the natural world. Weaving together archival research with memoir, Miles not only shares these diverse stories, but also puts forward an argument explaining why it’s so important for girls and young women to have equal access to the outdoors. —Jaime Herndon
American Scientist Comments and Discussion
To discuss our articles or comment on them, please share them and tag American Scientist on social media platforms. Here are links to our profiles on Twitter, Facebook, and LinkedIn.
If we re-share your post, we will moderate comments/discussion following our comments policy.