The Most Powerful Movements in Biology
By S. N. Patek
From jellyfish stingers to mantis shrimp appendages, it takes more than muscle to move extremely fast.
From jellyfish stingers to mantis shrimp appendages, it takes more than muscle to move extremely fast.

DOI: 10.1511/2015.116.330
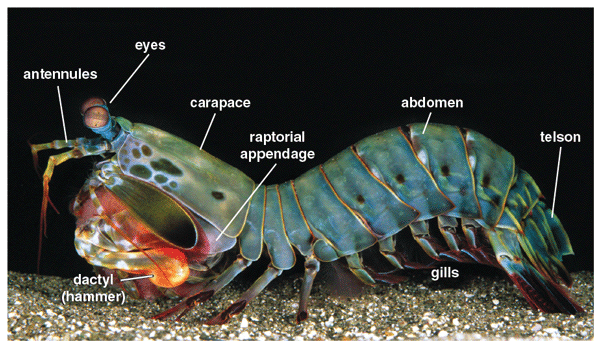
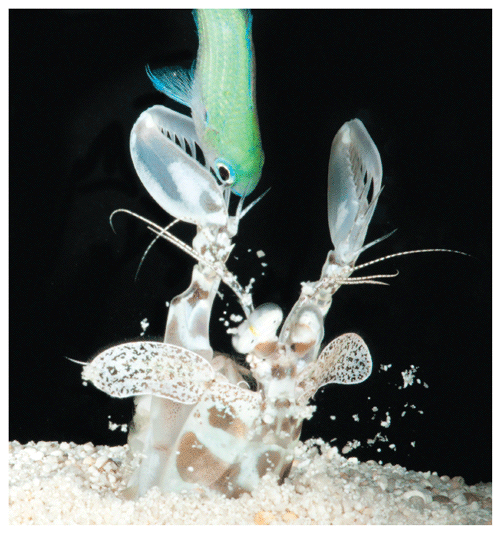
I began to observe colorful peacock mantis shrimp, predatory crustaceans that smash snails with a hammer-shaped appendage, when I was a postdoctoral fellow in Roy Caldwell’s laboratory at the University of California, Berkeley. The mantis shrimp’s process of breaking a snail was a delight to observe.
They probed, wiggled, and positioned a snail into place. Just before smashing the snail, they touched the snail’s surface with antennules, possibly to attain a sense of the position and surface of the target. After what anthropomorphically felt like an inhale before a dive, the mantis shrimp struck. The strike itself was invisible—too fast to see with the naked eye—but a loud pop occurred, and new shell fragments appeared on the substrate. Then, the cycle began again: probing, wiggling, positioning, touching, “inhaling,” and then, “pop,” another invisible but loud strike occurred. Silence reigned in the tank when the mantis shrimp finally began to eat the tasty morsel once protected by its shell. During these first observations, it never occurred to me that I was witnessing one of the fastest biological movements on the planet.
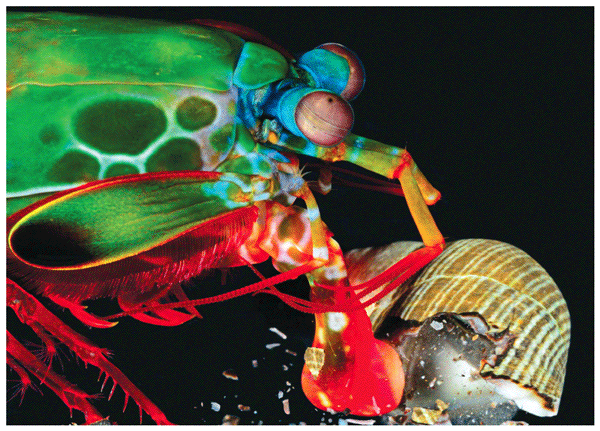
Photograph courtesy of Roy Caldwell.
I wanted to see and measure these “invisible” movements. After an arduous search to access a high-speed imaging system capable of showing me something more than just a blurred motion, I finally filmed strikes in slow motion. The images were so extraordinary that I knew on that first day of data collection that we had stumbled upon something remarkable. The movements happened within only a few frames even when filming at 5,000 frames per second—suggesting extreme speeds and accelerations. A brilliant bubble was visible between the hammer and the shell. Indeed, I soon realized that, contrary to my expectations, the fastest biological motions are not generated by cheetahs, the blink of an eye, or an escaping fish; instead, they occur in small, obscure creatures that have harnessed one of the great challenges in physics and engineering: extreme power output.
Over the subsequent years that I worked on extremely fast systems, this emerging field has yielded results that surprise and unsettle the standard expectations for what is “fast” in biology, while also offering treasure troves of information at the interface of biology, physics, and engineering. The realm of ultrafast life is populated by extraordinarily fast creatures, such as jaw-jumping trap-jaw ants, self-launched fungal spores, ballistic termite jaws, and stinging jellyfish. They challenge our assumptions about why organisms move fast and the costs that accompany such extreme capabilities. Mantis shrimp have received the most intensive examination of any system in this realm and are now a key system for probing the deep evolutionary history of extreme weaponry, the mechanical and evolutionary trade-offs accompanying extreme movement, and the technical applications of biological discoveries.
Once we began analyzing those first high-speed images of smashing mantis shrimp, the movements were far faster than anyone could have imagined. Their hammer-shaped mouthparts, called raptorial appendages, accelerate like a bullet in a gun (100,000 meters per second squared) and achieve speeds up to 31 meters per second that rival highway traffic moving at 69 miles per hour. The duration is so brief that more than 100 of these strikes could fit within one blink of an eye. A human needs to use a robust hammer-blow to break the same snails that these small crustaceans can fracture with raptorial appendages that are smaller than a child’s pinky finger.
Animal movement inevitably invokes the role of muscle, but it turns out that to achieve these extraordinarily powerful movements, organisms must actually find ways to circumvent muscle’s limitations. A simple analogy explains the conundrum. Imagine throwing an arrow at a target, just using your arm muscles. The arrow would not go particularly far or fast. However, if you use those same arm muscles to flex a bow and then release the arrow with your fingers, suddenly the arrow easily reaches and punctures its target. The energy input is the same whether or not a bow is used. The only difference is the time over which the energy is released. With just an arm muscle, the energy output occurs over a relatively long time period. With the addition of a bow, the energy release occurs over extremely short time scales. The result is power amplification—the crux of all ultrafast movements. Power is defined as work divided by time. By decreasing the time over which work is performed, power is amplified.
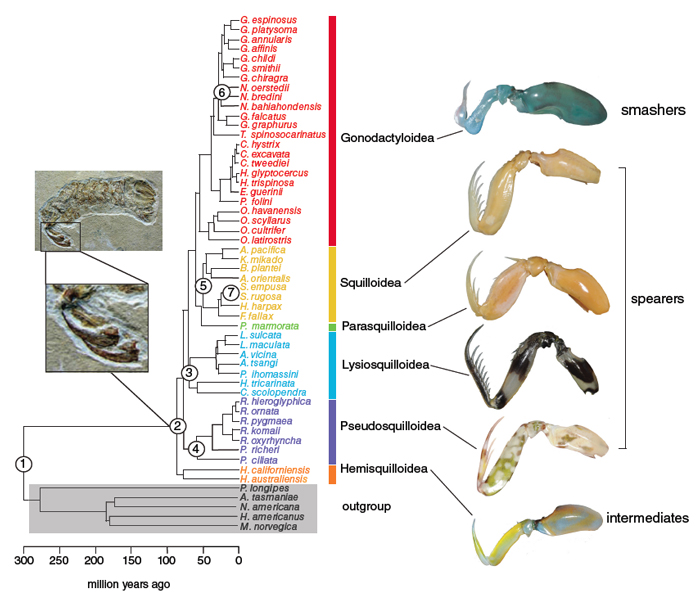
Figure adapted from T. Claverie and S. N. Patek, 2013.
Just like the bow and arrow example, mantis shrimp raptorial appendages contain a spring and a latch to generate extreme power amplification. Their mechanism for power amplification is just a tweak to the standard antagonistic muscle contractions that characterize most animals’ motor systems. Just like the extensor and flexor muscle pairs that extend and flex our limbs, mantis shrimp raptorial appendages use extensor muscles to swing out their hammer and flexor muscles to fold appendage segments toward the body during normal, daily activities. However, when they need to do a high-powered blow, they contract the flexor and extensor muscles simultaneously (similar to the antagonistic leg muscle contractions that we do prior to a jump). When they co-contract these muscles, the large, bulky extensor muscles compress an elastic system and tiny flexor muscles pull latch-like mineralizations of their apodemes (tendons) over a small lump inside the appendage, thus providing effective mechanical advantage over the high forces of the large extensor muscles. The result is … no movement at all! The system is primed to strike as soon as the flexor muscles relax, release the latches, and permit the stored elastic energy to release over an extremely short time period to push the hammer forward with extreme power output.
To varying degrees, this is the trick that all high-power systems use: They temporally and spatially separate slow loading and energy storage from the rapid release of energy that confers power amplification. Trap-jaw ants release tiny latches that block their preloaded mandibles (watch a video on Patek's research on trap-jaw ants). Two droplets slowly grow until the point at which they fuse over exceedingly short time scales to yield the power to launch a fungal ballistospore. The jellyfish’s stinger waits within a slowly pressurizing cell; a trigger hair dramatically releases the stored pressure and ejects the stinger toward its target. Thus, whether a muscle-based movement or a fluid-driven motion, the underlying mechanisms of ultrafast systems are all about power amplification.
The other remarkable feature of those first high-speed images of mantis shrimp strikes was the dramatic formation and collapse of a large bubble between the mantis shrimp’s hammer and its prey. I immediately recognized this bubble as a primary source of the popping noises in the lab: It was cavitation, a fluid dynamic process that happens during extremely fast movements in water. One region of water moving extremely quickly relative to adjacent regions yields low pressure that can form vapor bubbles. A paragon of power amplification, cavitation bubbles collapse over such short time periods that a massive, transient release of energy occurs in the form of intense heat (similar to the surface of the Sun), light, and sound. Engineers have had their own travails due to cavitation in fast-moving systems: Rapidly rotating boat propellers self-destruct due to cavitation bubble collapse, and fast-moving submarines generate loud noise from cavitation bubbles collapsing, which inevitably detracts from stealthy missions.
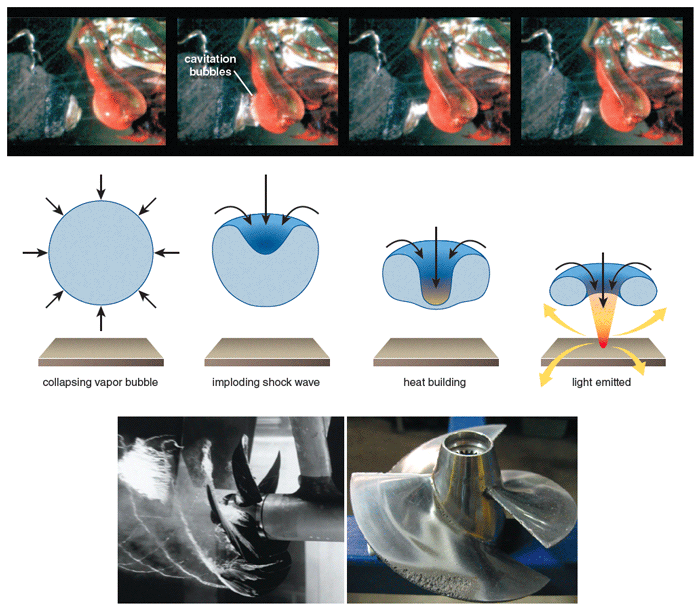
Top panel sequence from S. N. Patek and R. L. Caldwell, 2005. Illustration (center) by Barbara Aulicino. Photographs (bottom) courtesy of Wikimedia Commons.
While cavitation-based weaponry was already known to biologists through the curious cavitation bubble projectiles of snapping shrimp (distant relatives of mantis shrimp), the forces of cavitation had yet to be measured in these biological contexts. Intrigued as to whether cavitation bubble collapse generates measurable forces during mantis shrimp strikes, I developed an approach using piezoelectric sensors sampled at extremely high rates that ultimately detected the forces produced by both the impact of the appendage and those generated by the collapse of the cavitation bubble. This discovery yielded the first insights into the roles of impact and cavitation for high-speed prey capture in biology. In particular, we discovered that each ultrafast hammer blow by a mantis shrimp essentially strikes twice—once with the actual physical impact of the hammer and the second with the potent pressure waves of cavitation bubble collapse.
Photograph courtesy of Roy Caldwell.
Yielding rotational movements that rival the best-performing mantis shrimp, Suzanne Cox (a former graduate student in my laboratory, now at the University of Massachusetts Amherst) built Ninjabot, a physical model of mantis shrimp, to test the thresholds and conditions for cavitation and impacts during rapid rotation—a central issue for cavitation-resistant boat propeller design and ultrafast impacting systems. Ninjabot allows us to swap out real appendages with a variety of model shapes and materials to systematically test questions about fracture mechanics, materials, and cavitation. One intriguing finding is that mantis shrimp appendages don’t cavitate during ultrafast rotation, but when the appendages are attached to Ninjabot, they do cavitate. Thus, even holding the kinematics, materials, and shapes constant between a live mantis shrimp and Ninjabot, another factor seems to be suppressing rotational cavitation in mantis shrimp. The answer to this unresolved discovery may hold hints for designing propellers to reduce cavitation damage.
A mantis shrimp’s rapid-fire, high-impact, and cavitation-based assaults on snail shells occur with a substantial risk of damaging the mantis shrimp’s own appendage. Indeed, snail shells have been heralded as one of the most unbreakable materials in biology—yet mantis shrimp manage to crack them without fracturing their own appendages. Intrigued by this unusual ability, a research team led by David Kisailus at the University of California, Riverside, revealed the material composition and structural arrangement of the hammer that enables this impressive performance. They discovered that the outermost layer of the hammer is very hard and highly mineralized, primarily composed of concentrated phosphorus (for instance, calcium phosphate) and the typical crustacean material, calcium carbonate. Within the hammer, the materials are layered to dissipate energy and concentrate microcracks within the hammer rather than at its surface.
These discoveries of the structural principles of impact fracture mitigation in mantis shrimp appendages have already inspired new impact-resistant materials. Again from the Kisailus group, researchers used small chunks of carbon fiber–epoxy materials and shaped them into a helicoidal arrangement similar to the mantis shrimp’s hammer architecture. They then tested the impact and fatigue resistance of the new material compared to the mantis shrimp’s hammer at similar size scales. Ultimately, the materials inspired by mantis shrimp may be used in lightweight, high-speed impact systems for humans.
The challenges of wielding high-impact weapons are not unique to mantis shrimp. Each of these discoveries made through intensive analysis in this one model system has opened doors to more broadly considering the principles of ultrafast rotation in water, cavitation dynamics, and impact-resistant materials. Whether in engineered or biological systems, such as the impact-resistant materials of trap-jaw ant mandibles, microscopic puncturing spears in jellyfish, or cavitation bubble-wielding snapping shrimp, these early discoveries pave the way to more fully understanding the multi-disciplinary implications of the realm of the ultrafast.
It seems like any organism would benefit from extreme kinematic capabilities, but only a handful of ultrafast organisms have been documented. One obvious explanation for the small number of ultrafast creatures is that we have yet to discover all of them presently inhabiting our planet, given that these movements are invisible to the naked eye. Before filming mantis shrimp with extreme high-speed imaging, we certainly had no concept of their real capabilities. That initial and unexpected discovery in mantis shrimp has inspired our continued examination across many branches of the tree of life for as-yet undiscovered ultrafast creatures—leading to subsequent research on trap-jaw ants that jump with their ultrafast jaws as well as the near-invisible launching of fungal ballistospores. It is also likely, however, that a network of trade-offs guides and limits biological diversification, and that ultrafast systems come with some substantial limitations.
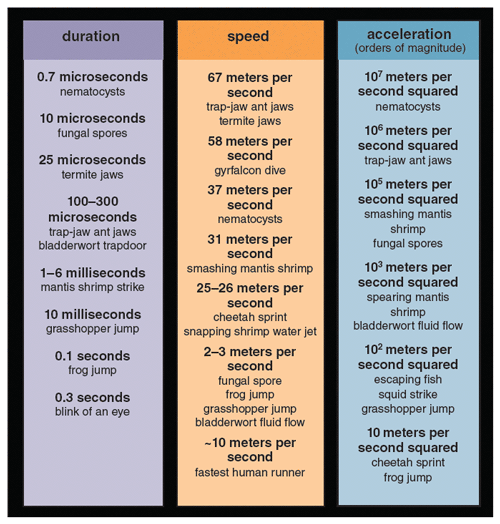
Illustration by Justin H. Storms.
Our first hint of broad underlying limitations on ultrafast systems came when we decided to film a different type of mantis shrimp than the hammering variety we initially studied. The evolutionary tree of mantis shrimp reveals that snail-smashing is the anomaly and that the large majority of mantis shrimp are spearers, which spear or stab evasive prey with elongated, spiny raptorial appendages that lack a hammer. Based on molecular and fossil analyses, smashers evolved from spearing mantis shrimp about 50 million years ago. After measuring the fascinating speeds of smashing mantis shrimp, my former graduate student Maya deVries (now at Scripps Institute of Oceanography) and I thought that we would find even more impressive kinematics in the spearers. That turned out not to be the case. In fact, spearers move at a small fraction of the speeds and accelerations of smashers.
The finding that fish-catching spearers move far more slowly than smashers was counterintuitive; we had expected that animals with the fastest weapons would be targeting the fastest prey. In fact, as we looked deeper into the habits of ultrafast creatures, we found that most do not target fast prey. Instead, the very fastest animals target defended, hard-shelled prey that typically do not quickly evade attack. If the biological machinery is present that could rapidly nab jumping or swimming prey, why wouldn’t ultrafast animals hunt evasive prey?
We had expected that the animals with the fastest weapons would be targeting the fastest prey.
One central trade-off of ultrafast systems—including mantis shrimp, trap-jaw ants, jellyfish stingers, and human engineered systems—revolves around the loss of control of the weapon once it is released. For example, when using a bow and arrow to hunt prey, the arrow is preloaded and aimed, but once the arrow is released, the archer cannot adjust its course and the arrow will only strike its target if the prey remained stationary. Ultrafast animals are so fast that underlying neurons cannot monitor or modify the movement once it has begun. Whether a trap-jaw ant, smashing termite, or a mantis shrimp, once they have released their ultrafast weaponry their neurons cannot send signals fast enough to relay and modify the system in real time. In an analysis of muscle activity prior to ultrafast movement, a former postdoctoral fellow in my lab (Katsushi Kagaya, now at the Seto Marine Laboratory in Japan) demonstrated that mantis shrimp vary strike velocity through modifications to muscle activity during spring loading, but once the strike begins the movement is too fast to permit adjustments by the nervous system.
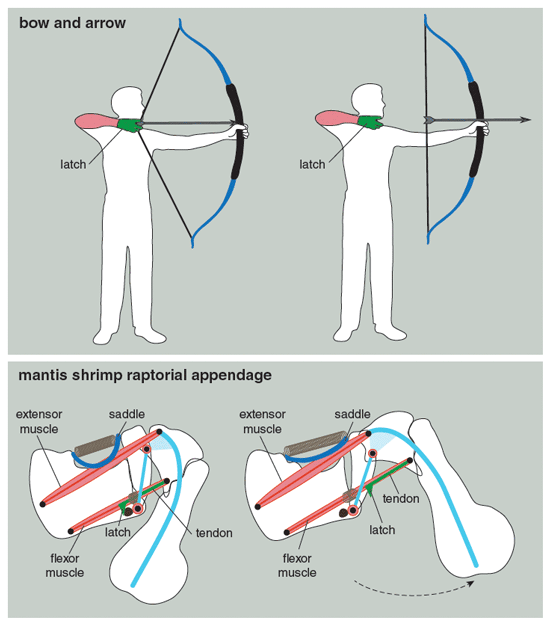
Illustration by Barbara Aulicino.
It takes a lot of time to be ultrafast.
Another biology-specific trade-off for ultrafast systems is almost a brain-teaser: It takes a lot of time to be ultrafast. Coming back to the principle of extreme power amplification, the key features are stored potential energy (typically in springs) and rapid energy release (through a latch). This means that energy is stored in advance and released extremely quickly. For ultrafast systems that use muscle, this trade-off is especially apparent. Muscles cannot contract both forcefully and quickly. The fundamental building block of muscle—the sarcomere—contains the proteins myosin and actin that bind together to generate the canonical striated muscle contraction. With longer sarcomeres, more actin–myosin bonds can be formed at a given instant, and the overall force of the muscle increases. However, if more bonds are formed at a given instant, then the rate of bond formation and release decreases, resulting in a slower muscle contraction. In sum, longer sarcomeres permit more force by a muscle but at a slower contraction rate.
Photograph courtesy of Roy Caldwell.
Making use of the evolutionary diversity of mantis shrimp raptorial appendages, a former undergraduate in my lab (Marco Mendoza Blanco) and I showed how the universal force-velocity trade-off in muscle plays out in ultrafast systems. We found that regardless of whether they are spearers or smashers, mantis shrimp have relatively long sarcomeres in the muscle that loads the spring, meaning that they have force-modified muscles that are good for loading stiff springs. However, the spearing mantis shrimp that target evasive prey have shorter sarcomeres than smashers, by up to 50 percent. Although the behavioral data have yet to be collected, the morphological data suggest that smashers evolved longer sarcomeres to compress more forceful springs and thus wield a potent strike, but at the cost of the rate of loading the system. In other words, smashers take a long time to load their weaponry, whereas spearers are faster at the draw. Ultimately, this may mean that the fastest animals cannot load their weaponry quickly enough to capture evasive prey, thus, counterintuitively, the predators of evasive prey can respond more quickly, but move at slower speeds. Simply put, it takes longer to be faster, and any muscle-based ultrafast system will encounter this trade-off during evolutionary diversification and thus potentially limit the broader use of ultrafast systems in biology.
Reflecting these significant trade-offs in ultrafast systems, our large-scale evolutionary analyses of mantis shrimp morphology again revealed that achieving extreme kinematics comes at a cost. In collaboration with a former postdoctoral researcher in my lab, Thomas Claverie (now at University of Montepellier), we found that the rate of morphological change in smashing raptorial appendages is slower than in other mantis shrimp. Associated with this decreased rate are more tightly coordinated changes among the mechanical components in smashing mantis shrimp compared to spearers. The physical demands of a tightly integrated ultrafast mechanism in smashers may well have reduced the inherent variability of the components, thereby reducing the potential for evolutionary change. Reduction of the potential for evolutionary diversification is a hefty cost for an ultrafast biological system and certainly offers a counterpoint to the easy, superficial notion that ultrafast systems are a pinnacle of design.
One last trade-off is perhaps the ultimate one: Ultrafast weapons are often lethal, and for populations and species to survive in the long run, organisms must develop strategies to avoid or reduce their use against conspecifics. Again, our model system of mantis shrimp offers some lessons. Mantis shrimp are essentially soft-bodied creatures, other than their raptorial appendages and their telson (armored tailplate), such that a well-aimed blow is very likely to be lethal. However, smashing mantis shrimp resolve their conflicts through a ritualized behavior in which they strike each other’s telson. A former postdoc in my lab, Jennifer Taylor (now at Scripps Institute of Oceanography), discovered that the striking hammer and receiving telson interact with similar dynamics to an ash bat hitting a baseball and that the energy returned to the hammer scales with the size of the receiving animal. One tantalizing possibility is that mantis shrimp actually assess each other’s size through the impact dynamics of this ritualized fight. Little is known about the reduction of conflict in animals with ultrafast weapons beyond these studies of mantis shrimp. Perhaps further studies of the ultrafast dynamics of lethal weapons in these and other animals will reveal novel behavioral and mechanistic pathways to de-escalating human conflicts.
Compared to the day when we obtained the first views of a mantis shrimp’s strike and started to peel back the layers of quirky details and broad principles of ultrafast organisms, this new realm of biology has developed into an intensely multidisciplinary field with a particular relevance to human systems and engineering design. As the field moves forward with hopeful anticipation for new discoveries of ultrafast creatures, the most significant data set for connections to engineering principles is the deep evolutionary history of these systems. Evolving for millions of years and leaving behind a fascinating fossil record that directly documents diversifying appendages over time, the mantis shrimp offer a natural experiment in engineered systems under a wide range of historical and present-day conditions. The data set includes stunning variants of weaponry, modifications of spring shape and function, trade-offs in muscle performance, and habitats including mud, sand, and live coral from the intertidal down to ocean depths.

Photographs courtesy of Roy Caldwell.
This diversity of structures, systems, ecology, and time periods offers a matrix of variables that can be mined for combinations of traits that work best under particular conditions. Trap-jaw ants also exhibit extraordinary evolutionary diversity; in their case, at least four independent evolutionary origins led to ultrafast mandibles, thus offering a data set of the conditions for and consequences of the origins of ultrafast mechanisms. Fungal ballistospores are found across a massive number of species with a diversity of shapes and habitats that can inform the dynamics of droplet propulsion systems. Similarly, snapping shrimp and jellyfish stingers exhibit fantastic diversity of mechanisms and morphology.
From the behavioral dynamics of ritualized fighting to the stochastic challenges of cavitation avoidance, these powerful yet small creatures have opened many unanticipated windows into physics, evolution, engineering, and ecology. This world of discoveries was revealed through breakthroughs in imaging technology that now readily permit scientists to examine extremely fast movements and extraordinarily high power biological systems. With discoveries of new ultrafast systems on the horizon, combined with deeper investigations into basic and applied science, this remarkable realm of biological capabilities has newly emerged as an exciting, multidisciplinary field.
Click "American Scientist" to access home page
American Scientist Comments and Discussion
To discuss our articles or comment on them, please share them and tag American Scientist on social media platforms. Here are links to our profiles on Twitter, Facebook, and LinkedIn.
If we re-share your post, we will moderate comments/discussion following our comments policy.